Virtual Care 2.0
I recently had the opportunity to participate in NCQA’s Health Innovation Summit along with 1,300 leaders, clinicians, and professionals from across the healthcare ecosystem. The four-day event featured insights about topics such as “Hospital @ Home” and “On Demand” clinical services, and showcased innovators involved in: diabetes remission through technology-enabled behavior change, the transition to digital measurement of quality, and health equity (to name just a few!).
I share a few highlights here from the talk my colleagues and I gave about the transformation to Virtual Care 2.0:
- My colleague Erkan Hassan , Pharm.D, FCCM highlighted clinical studies about the efficacy of telehealth in the acute care setting, including tele-ICU care, as well as with remote patient monitoring and hospital at home efforts currently underway.
- My colleague, Joe McMenamin, M.D., J.D. highlighted the key considerations for telemedicine post-Public Health Emergency (PHE). He focused on legal considerations such as professional licensure, provider-patient relationship, privacy, liability, and reimbursement; noting how the anticipated end of the PHE will impact these.
- My focus was on the leadership dimensions of this transformation to a virtual care world.
LEADING TRANSFORMATIONAL CHANGE
As health and human service organizations embark on their Virtual Care 2.0 approach, I encourage leaders to consider these key ingredients for leading this transformational change:
A Compelling Vision
Leaders are well-served to define the strategic, clinical and business case for virtual care. My collaborating partner Christian Milaster writes about that here.
With clarity about the Why, leaders can share a more compelling and clear vision for the future of virtual care in your organization.
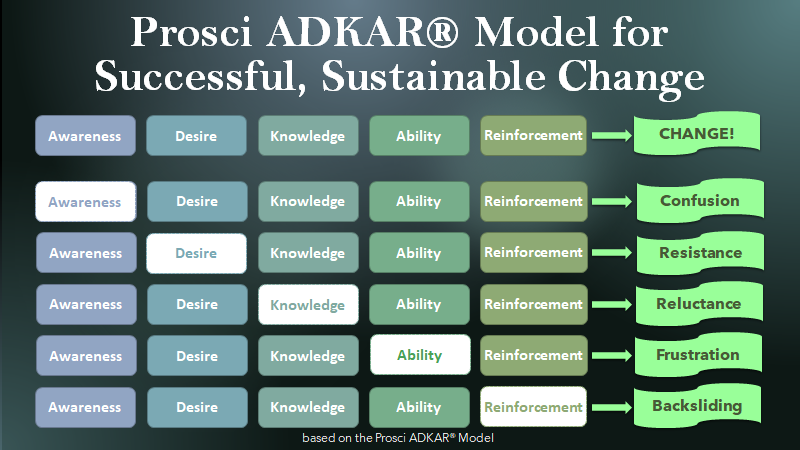
Without awareness of the Why, or desire, providers and staff will become confused and resistant to change including to changes that involve additional types of virtual care services.
A Clinical Champion, with time allocated!
Virtual care and telemedicine are first and foremost a clinical service. As such it is key to have a Clinical Champion at the helm of (or least in a key guidance role for) each of your virtual care endeavors.
They, of course, need to be supported by other capable professionals. However, I strongly encourage that your Clinical Champion has time allocated to oversee, guide, and advise on your virtual care services. If in name only, your services may not gain clinical acceptance and therefore long-term success.
True leadership with a strong base of supporters
Moving beyond the basic video visit, into other realms of virtual care, organizations should consider the base of supporters, influencers, and leaders needed to design, launch, expand, monitor, promote, and improve these new clinical service offerings. Support is needed in clinical, operational, financial, and technical dimensions.
Without high quality education and training to build the competence and confidence (!) of each clinician and all staff involved in virtual care services, we understandably see reluctance and frustration.
If you are hearing “my patients don’t want telehealth,” I strongly encourage you to look under the hood at the training (or lack of such) that has been provided to your clinicians. Without confidence in diagnosing and providing care via new delivery modes (such as tele-exams with clinical tools, or patient monitoring from a distance), your clinicians will not like virtual care, and by extension neither will their patients.
Clinicians do not want to look inexperienced in front of their patients. Who can blame them!
And they do not want to be the ones to “troubleshoot” technical issues. And who would want them to!
But without ample virtual care training and ongoing support to clinicians and their patients, we repeatedly hear of immense frustrations. It does not have to persist this way; many are focusing on first optimizing what they rapidly stood up in 2020.
Elevating successes and early adopters
It is wise to shine a light on early success cases such as patient situations where the outcomes were positively impacted by virtual care access. These early successes can be in similar organizations, or even better if from your own.
For instance, I was struck by cases presented at the Innovation Summit by physicians where they noted good outcomes with shorter periods of “hospital-level” care for patients in their Hospital at Home program as compared to similar patients receiving care in brick-and-mortar inpatient hospital settings.
I also find great value during a transformation to demonstrate visible support for the early adopters. Their example can serve as role models for others who are still in the watching and waiting mode.
Measuring and sharing results
One of several ways to ensure continued success in your organizational transformation is by measuring, monitoring, and then improving upon your results.
Define your key performance metrics for these new clinical services and monitor them closely. This will highlight aspects needing tweaking or retooling.
Over time, the results will tell the true story of your transformation.
If you’d like to receive these Inspirations in your inbox every other week, you can subscribe to Kathy’s Excellence Advantage Inspirations Newsletter.
Kathy Letendre, President and Founder of Letendre & Associates, advises organizations and leaders to create their excellence advantage.
Contact Kathy by phone or text at 802-779-4315 or via email.

