Virtual Care: From Strategy to Action to Results
Whether you work within the healthcare ecosystem or experience it as a patient, we can all agree that the past few years have brought immense change.
In what was once exclusively a brick-n-mortar industry – with all its related complexities and inconveniences – the pandemic has challenged many to think differently and consider where virtual care can improve outcomes for patients. We are reimagining possibilities, revisiting long-held assumptions, and enacting new strategic approaches.
During the public health emergency, with an easing of restrictions and payment structures, telehealth was thrust into the spotlight almost overnight. For some organizations this chaotic entry into virtual care is where they started…and unfortunately, for many, where they still reside today! For these organizations, they equate telehealth with occasional video visits or phone calls to patients.
For other organizations, their rapid learning experience in 2020 has now catapulted them into a strategic position. For them, hybrid and virtual care are a growing part of their service offerings. They are focused on serving patients in hard to reach areas. They are equipping members of their communities with access points, digital navigators, and other supportive means. They have expanded beyond video visits, and are embedding virtual care modalities such as wearables, remote patient monitoring, and texting into their care approaches.
Many of you are aware that I am a frequent collaborator and contributor with Ingenium Digital Health Advisors.
Ingenium’s telehealth maturity model has helped many organizations to determine where they are and most importantly to establish where they need to be to succeed with virtual care:
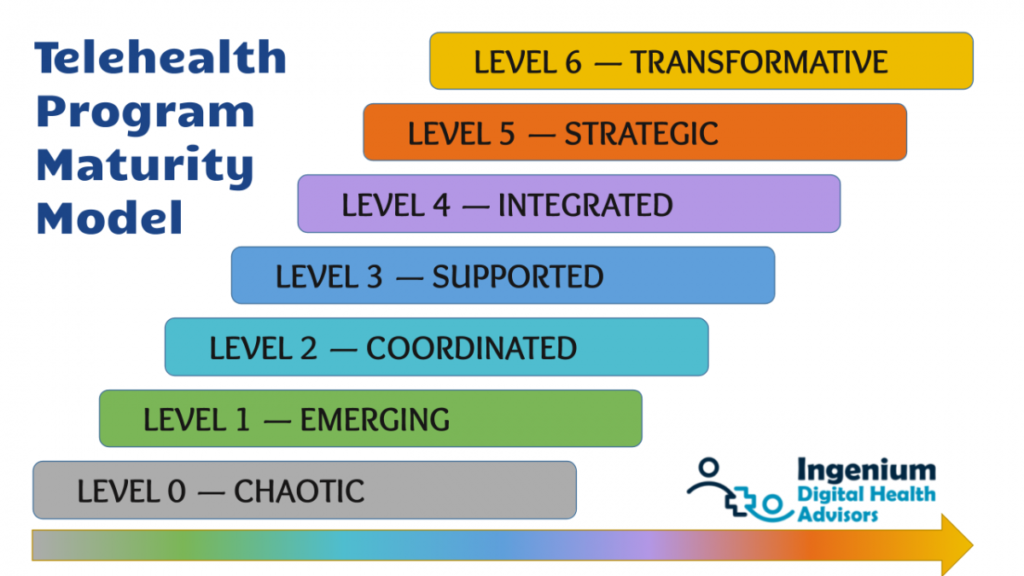
I offer a few illustrative examples of organizations who have moved beyond coordinated into the strategic realm (and beyond):
One behavioral health organization was already dabbling in telehealth pre-Covid. Further, they had defined virtual care as a key strategic priority for 2020-1. When the world went into lock-down they went into ramp up. They invested in solidifying their telehealth program with a telehealth steering team and designated coordinator, focused on clinician engagement and confidence, and put in place the routine monitoring of performance indicators. They sought expertise to get this in place well. After reaching the “Integrated” level of maturity, they set their sights on the Strategic level by broadening from telehealth into digital health. They are now partnering with innovators to explore and introduce digital modalities to best serve their client populations.
Another organization, a personalized primary care practice, has been increasing its use of digital tools to coordinate care, personalize the patient experience, and manage more efficiently. They are early adopters in the use of technology-based tools to avert unnecessary admissions and ER visits. They are seeking to transform how primary care is delivered to their patients. Their business model is evolving due to keen interest in their results.
A third organization, serving a very large geographic area, is using virtual care to reach residents across their region who have transportation challenges. They are expanding two key service lines where frequent appointments are essential for clients’ recovery. They are simultaneously converting cancellations into virtual care appointments. They are moving from emerging to integrated through thoughtful planning, solid workflows, attention to barriers for patients, and tailored clinician engagement.
A fourth organization recognizes that relying on localized staffing for all services is no longer necessary in the virtual model. They are broadening their team by augmenting their highly skilled local staff with virtual team members. They are widening their virtual care strategy not only from a quality and patient experience perspective but also from a workforce perspective.
And lastly, is another example, that I am immensely proud to be a part of. This is a four-county convening organization that is advancing virtual care across a vast, rural region through a multi-faceted approach. Having set a region-wide strategy for virtual care, they are:
- bolstering the telehealth capabilities of numerous clinical partners;
- establishing library-based access points in the first of 30 branches;
- setting up “neutral” access points in schools for students, staff, and eventually families where various primary care, behavioral health, and specialty care providers will be able to connect with those needing services;
- partnering with other entities in the region to improve digital literacy, provide devices and minutes to those without the means to obtain on their own, and establishing a cadre of digital navigators in community settings; and
- monitoring the impact of all of the above through a multi-year telehealth impact assessment.
This approach is and will be transformative for the region.
These are just a handful of examples of moving from strategy into action into results with virtual care.
Here are a few additional and useful resources from my colleague, Christian Milaster, on the Ingenium maturity model for telehealth, including a self-assessment.
If you’d like to receive these Inspirations in your inbox every other week, you can subscribe to Kathy’s Excellence Advantage Inspirations Newsletter.
Kathy Letendre, President and Founder of Letendre & Associates, advises organizations and leaders to create their excellence advantage.
Contact Kathy by phone or text at 802-779-4315 or via email.

